BEE VENOM TREATMENT FOR ASTHMA
|
Asthma and Its Expression
Asthma has affected a large population that includes adults and children. This disease is more common in the developed and industrialized world. It has been observed that during the past 50 years the cases of asthma have significantly gone up. Talking about the west, it can be said that nearly 10% of the general population suffers from asthma and among those affected, the percentage of boys is greater than of girls. |
What Is Asthma?
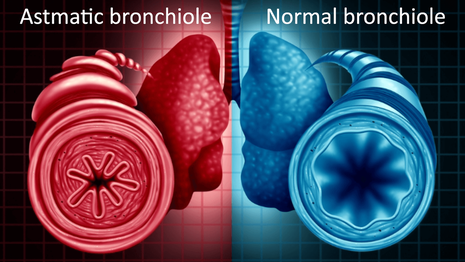
Asthma is a type of chronic inflammation that contracts muscles present around the trachea and leads to swelling of the mucous membrane. What does that mean? To be clear, asthma restricts the normal flow of air to lungs and that leads to shortness of breath, wheezing and coughing. Furthermore, the patient of asthma experiences sinus and nasal problems along with slimming in the chest. These are the basic symptoms of asthma.
What Are The Possible Triggers Of Asthma?
In several cases of asthma, these symptoms can get quite severe and if not dealt with on time, they can lead to severe consequences. It has to be determined yet that what causes asthma, but it is generally believed that certain chemicals, poor indoor environment, allergies, and air pollution can trigger asthma. Some people also have heredity asthma. It happens when one or both of the parents have symptoms of asthma. As a result, it is quite likely that their child will also develop symptoms of asthma at some point.
Who Suffers From Asthma?
Asthma can affect children too and the good thing is that symptoms can fade away with time. There are two different types of asthma: non-allergic asthma and allergic asthma. Adults usually face symptoms of non-allergic asthma, while children mostly suffer from allergic asthma.
It is also to be understood that allergic asthma can easily develop in those patients, who have some sort of hypersensitivity related to mites, animal fur, and pollen. When the body experiences any of these triggers the antibodies come into action that leads to an allergic reaction, which is called asthma.
On the other hand, non-allergic asthma is usually triggered by different respiratory infections, physical exertion, exhaust gases, tobacco smoke, perfume, drugs, cold air, smog, and dust.
A subject of asthma must judge the condition and make use of the latest and effective natural treatments like honey bee venom to control the symptoms. Any sort of treatment takes some time to deliver its effects so, patience is requested.
Protective Effects of Intratracheally-Administered Bee Venom Phospholipase A2 on Ovalbumin-Induced Allergic Asthma...
Therapeutic options that are currently being used to control symptoms of asthma include β2 agonists and corticosteroids. Both of these treatments are effective in controlling the harmful side effects of asthma.
For this study, one of the main elements of BV (bee venom), the characteristic of PLA2 (phospholipase A2) was examined carefully. A clinical model of asthma was chosen for this reason and it was considered that how PLA2 helps in reducing inflammation of the airways and improving lung functioning.
Female BALB/c mice were chosen for the experiment and they were induced with allergic asthma. Intraperitoneal injection of OVA (Ovalbumin) was administered on the 1st day and the 14th day of the clinical study. OVA was followed by an intratracheal trial having 1% OVA given 6 times during the 22nd and 30th day of the treatment.
During this time, lung histology and infiltration of the immune cells like Th2 cytokines in lungs were evaluated in OVA administered female mice in the company and nonattendance of an intratracheal trial of bee venom PLA2.
Results showed that intratracheal trials of bee venom PLA2 lead to suppression of OVA-induced allergic asthma in female mice. Airway inflammation was managed due to a reduction in AHR. It also helped in reducing goblet cell hyperplasia. In addition to that effect, it was noted that there was a prominent decrease in the production of Th2 cytokines like IL-13, IL-5, and IL-4. Furthermore, the total number of cells that included neutrophils, macrophages, and eosinophils in the airways were also brought down.
Bee Venom Phospholipase A2 Suppresses Allergic Airway Inflammation In An Ovalbumin‐Induced Asthma...
For a long time, bee venom therapy has been used in different forms and combinations to deal with chronic inflammatory diseases. Bee venom has been regarded, as one of the best alternative medicines for respiratory tract issues. It has been already demonstrated that bee venom boosts natural immune tolerance by increasing the amount of Tregs (T cells) in different immune system disorders.
But still, it needs to be determined how bee venom helps regulate this specific response of the immune system. In this clinical study, it was deeply investigated how bee venom PLA2 supports positive effects that are delivered via T-cells in different models of asthma. Bee venom PLA2 was given to OVA challenged mice through intraperitoneal injection. During this study, developments and behavior of the OVA challenged mice were studied in terms of lung histology, Th2 cytokines, Treg population and differential, and total bronchoalveolar lavage fluid cell count.
Treg depletion was observed to assess the reduction of symptoms related to asthma and Treg migration. Dependence of CD206 on bee venom PLA2 treatment that leads to suppression of the airway inflammation in OVA challenged mice was also evaluated in the due course. Bee venom PLA2 treatment helped induce Tregs that ultimately brought down the infiltration of the inflammatory cells in the lungs of OVA challenged mice. It was observed that Th2 cytokines, present in BALF (bronchoalveolar lavage fluid), were reduced significantly in the mice treated with bee venom PLA2.
But the reduction of inflammatory cells, after administration of bee venom PLA2, after the OVA challenge was not observed in the Treg depleted mice. Furthermore, it was also investigated that what type of involvement is controlled by CD206 in the bee venom PLA2 treated OVA challenged asthmatic models of mice.
According to the clinical assessment, there was an impressive reduction in the levels of inflammatory cells and TH2 cytokines in the bronchoalveolar lavage fluid of those OVA challenged mice that were treated with bee venom PLA2. But the Ova induced and bee venom PLA2 CD206 mice did not show this positive response. In the light of this clinical observation, it can be easily said that bee venom PLA2 can alleviate inflammation of the airways by inducing Tregs in the OVA challenged asthmatic models of mice.
6 Male C57BL mice, 6 to 7 weeks old, were obtained from the Charles River Korea, Orient Bio, Korea. While the CD206 mice (B6.129P2‐Mrc1tm1Mnz/J, Foxp3EGFPC57BL/6 mice, and Foxp3EGFPBalb/c (C.Cg‐Foxp3tm2Tch/J) mice were obtained from the Jackson Laboratory, Bar Harbor. All of the model mice were provided with air conditioning and a proper 12 hours based light and dark cycle along with pathogen-free conditions. They were also given access to food and water to make sure that they remain healthy during a clinical study. The method adopted for conducting lab research on the mice was by the specified Rules for Animal Care and the Guiding Principles for Animal Experiment Using Animals that were acknowledged by the University of Kyung Hee Animal Care and Use.
Model mice were prepared for the study through intraperitoneal injection having aluminum hydroxide 20mg and ovalbumin, which was given on the 1st and the 14th day. Mice were also intratracheally challenged with only 1% of OVA given 6 times between the 20th and 31st days. On the other hand, negative control mice were challenged and prepared with PBS alone. Bee venom PLA2 challenged group was treated with 0.2mg/kg bee venom PLA2 intraperitoneal injection after every three days between the 3rd and 17th day. A fresh lab experiment was carried out after a passage of 24 hours of administration of last intratracheally OVA challenge.
Levels of IFN-γ, IL-13, IL-5, and IL-4 in BALF were evaluated with the help of the BD Biosciences System meant specially for assessing the level of these factors through the quantitative sandwich enzyme-linked immunoassay kit. Level of serum OVA-specific IgE and simple IgE was gauged through ELISA. After administering anesthesia to mice, samples of blood were collected from their retro-orbital plexus. The centrifugation method was used to obtain serum samples. Those were stored at minus 20-degree centigrade until assay. To measure the IgE levels, stored samples of serum were diluted with 5% FBS in assay diluent.
On the 31st day of clinical examination, mice were thoroughly analyzed with the help of a noninvasive lung functional measurement method to calculate the AHR. Model mice were placed inside the barometric plethysmographic chamber for three minutes to obtain baseline readings.
Statistical analysis of all the data samples collected was conducted with the help of Prism 5 Software obtained from Graph Pad Software Inc., CA, USA. Any sort of Differences between treatment samples and means of control were examined through one way ANOVA from Turkey’s Multiple Comparison Test.
According to the studies carried out earlier, it was determined that the percentage of Tregs rose significantly in the bee venom PLA2 treated splenocytes when compared with PBS treated cells. Recent reports suggest that the Tregs can help suppress hyperresponsiveness and airway inflammation in asthma model mice. To define the role of bee venom PLA2 for inducing Treg cells to the airway, the percentage of Treg cells present in lung tissues was calculated in the OVA-induced asthma mice.
Inoculation was given twice, to the mice with the OVA on the 1st and 14th day of the clinical study. Right after 6 days of second immunization, mice were intratracheally challenged through 1% OVA that was given for 6 times between the 20th and 31st day. It was found that the Treg population did not change in the OVA group when compared with the CON group. On the other hand, the Treg population showed an impressive rise in the bee venom treated OVA group.
Treg population in Treg depleted mice did not show any significant change after receiving bee venom PLA2 treatment. The reason being, the effects of the anti CD25 antibody injection were already present in those mice. After this the mRNA profile of the lung tissues from PLA2 + OVA, OVA and WT treated mice were examined to evaluate secreted production of PLA2 in the OVA-induced asthmatic mice. It was found that there was no increase recorded related to Spla2-V and Spla2-IID in the OVA+PLA2 and OVA-induced mice when compared with the WT mice.
After OVA challenge the total lymphocytes, macrophages, neutrophils, eosinophils and cells in BAL fluid had gone up and that clearly shows that induction of allergic asthma in the mice was successful. It was also noticed that inflammatory cells had gone down after bee venom PLA2 treatment. However, a similar effect was not recorded in the Treg cell-depleted group. Though Th2 cytokines were lowered after bee venom treatment in the OVA-induced model of asthmatic mice.
Histological analysis of the lung tissues from the OVA group of mice demonstrated an excessive rise in inflammatory cells located in the lung parenchyma. The CON group didn't show any alarming rise in the inflammatory cells. Bee venom PLA2 therapy also controlled the manifestation of inflammatory cells and lowered down the population of the PAS-positive goblet cells located around the bronchial airway. However, neither the appearance of MYL9 nor the number of PAS-positive goblet cells was changed by bee venom treatment in the Treg depleted mice.
Summarizing the lab research done on different models of asthmatic mice group, it can be declared that administering a controlled and formulated; bee venom PLA2 treatment can help control symptoms of allergic asthma. BvPLA2 is an effective source for regulating Tregs in the bronchial airways. It can also be said that the Treg population that was induced with bee venom PLA2 treatment is directly linked with the CD206 that ameliorates allergic inflammation.
Still, further study is required to refine and define the involvement of the molecular mechanism that is involved in the bee venom PLA2-CD206 process. It could help in developing an effective therapeutic strategy for treating patients of asthma – without any serious side effects.
Sources:
Protective Effects of Intratracheally-Administered Bee Venom Phospholipase A2 on Ovalbumin-Induced Allergic Asthma...
Bee Venom Phospholipase A2 Suppresses Allergic Airway Inflammation In An Ovalbumin‐Induced Asthma...